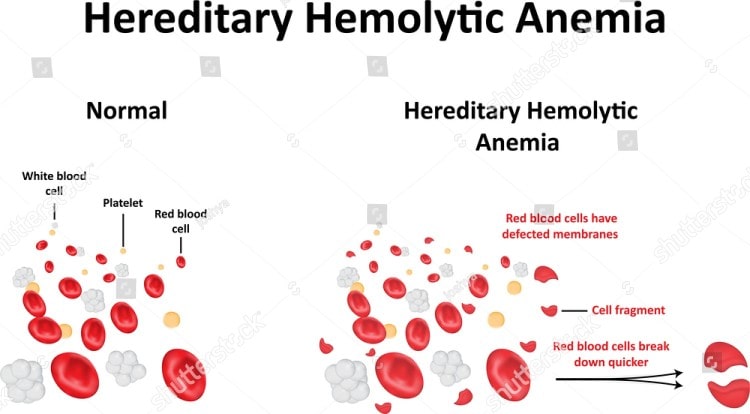
Hemolytic anemia is defined as a reduced amount of red blood cells in the bloodstream due to the abnormal breakdown of these cells either in the blood vessels or elsewhere in the body, such as the spleen. The classification of hemolytic anemia can be categorized into either inherited or acquired causes and the treatment of the condition will depend on these factors.
In a healthy individual, the rate of red blood cell breakdown in the body is every 90 to 120 days and the spleen is the organ that removes the old and damaged cells in the bloodstream. In cases of hemolytic anemia, certain conditions cause the red blood cells to break down faster than the body can produce them resulting in anemia.
Causes1
Inherited
Also referred to as intrinsic causes, where the issue is related to the red blood cells themselves, the following are conditions that may result in inherited/hereditary hemolytic anemia:
- Sickle-cell disease, thalassemia, and congenital dyserythropoietic anemia which cause defects in the production of hemoglobin.
- Hereditary elliptocytosis and hereditary spherocytosis which are associated with defects in the production of the red blood cell membranes.
- Pyruvate kinase deficiency and glucose-6-phosphate dehydrogenase (G6PD) deficiency which causes defects in the metabolism of red blood cells.
- A rare hereditary cause of hemolytic anemia also includes paroxysmal nocturnal hemoglobinuria (PNH) which is a potentially life-threatening condition.
Acquired
Also referred to as external or extrinsic causes, where red blood cells are mechanically damaged while circulating throughout the body, the following conditions are associated with acquired causes of hemolytic anemia:
- Conditions affecting the immune system – these include temporary issues such as a Mycoplasma pneumonia infection resulting in cold agglutinin disease or more permanent problems such as autoimmune hemolytic anemia. The latter is more commonly present in conditions such as rheumatoid arthritis, lupus, chronic lymphocytic leukemia, and Hodgkin’s lymphoma.
- Any cause of an overactive spleen (hypersplenism) such as portal hypertension, for example. When there is increased activity of the spleen, there is an increased breakdown of red blood cells.
- Spur cell hemolytic anemia that is caused by liver disease. If the liver doesn’t function properly then free cholesterol bonds to the red cell membrane causing the cell to rupture.
- Certain infections, such as malaria, can increase the chances of hemolytic anemia, especially in those patients who have sustained burns.
- Certain poisons and toxins such as lead, stibine, or arsine can lead to non-immune hemolytic anemia.
- A low-grade hemolytic anemia may occur in around 70 percent of patients who received prosthetic heart valves and severe hemolytic anemia occurs in 3 percent of these patients.
- A condition known as “footstrike hemolysis” may occur in runners where they develop hemolytic anemia as a result of red blood cells being destroyed in their feet due to the impact on the heels.
Signs and Symptoms
In general, the signs and symptoms of anemia include demonstrating a pale skin, and fatigue. In severe cases, patients may present with a rapid heartbeat, heart palpitations, shortness of breath, a low blood pressure, confusion, and even loss of consciousness. The reason why patients exhibit these issues is that when red blood cells are destroyed the protein hemoglobin can no longer transport oxygen to the cells, tissues, and organs that require this gas in order to function properly.
In hemolytic anemia, since the red blood cells are broken down, their contents spill into the bloodstream and this includes a product known as bilirubin. This bilirubin circulates in the bloodstream causing the skin and/or eyes to appear yellow in color and this is called jaundice. If an individual has chronic hemolysis, then enough bilirubin can be excreted into the bloodstream to result in the development of gallstones in the gallbladder.
Free hemoglobin is also released into the bloodstream and if this becomes a persistent issue then the affected individual may develop increased pressure in the blood vessels supplying blood to the lungs (pulmonary hypertension). In turn, this leads to fainting spells, severe shortness of breath, and chest pain and the condition can complicate to right heart failure. As a result, right heart failure can lead to fluid accumulation in the soft tissues of the legs (peripheral edema) and the abdominal cavity (ascites) and this can lead to left heart failure. The presence of both conditions is then referred to as congestive heart failure.
Reference
1. Guillaud C, Loustau V, Michel M. Hemolytic anemia in adults: main causes and diagnostic procedures. Expert Review of Hematology. 2012 Apr;5(2):229-41. doi: 10.1586/ehm.12.3.